Ogilvie syndrome aka colonic pseudoobstruction
- related: GI
- tags: #GI
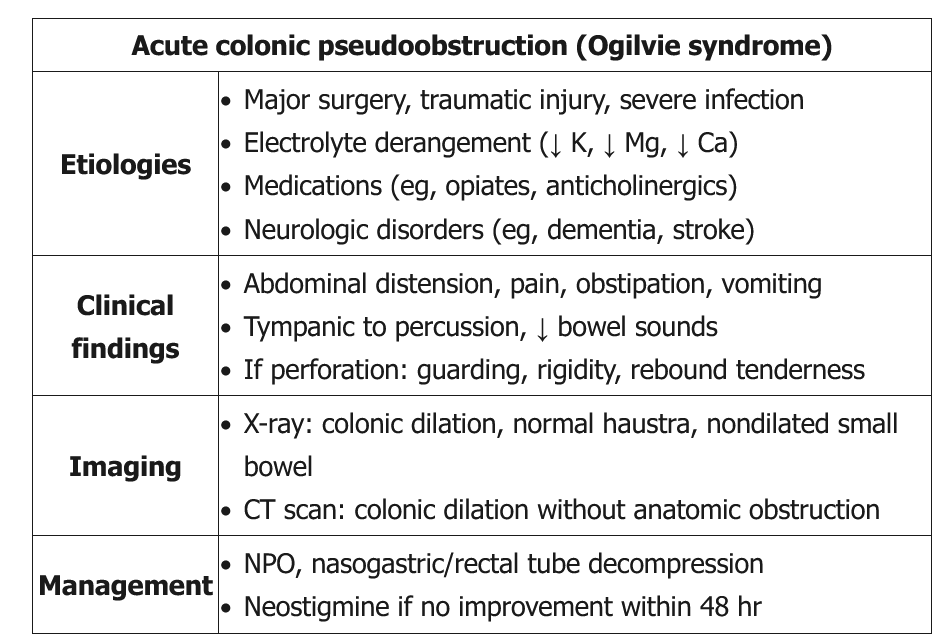
Ogilvie syndrome is most common in hospitalized or institutionalized men age >60. Although its etiology is unclear, it is suspected to be related to autonomic nervous system dysfunction in the setting of prior insults (eg, trauma, surgery, infection, neurologic disorders), particularly in combination with metabolic abnormalities (eg, hypokalemia, hypomagnesemia) or inciting medication (eg, narcotics). Patients typically have abdominal distension, pain, nausea/vomiting, constipation, or diarrhea. Examination commonly reveals a distended abdomen with increased tympany, mild tenderness, and active bowel sounds; peritoneal signs are suggestive of perforation.
CT scan is diagnostic and can differentiate Ogilvie syndrome from mechanical obstruction (presence of transition point) and toxic megacolon (thickened colonic wall with thumbprinting). Treatment is initially supportive. Serial abdominal examinations and x-rays should be performed to evaluate for perforation. In addition, management includes nasogastric tube decompression, treatment of possible underlying causes (eg, electrolyte imbalances, narcotic cessation), and early ambulation.
Neostigmine is indicated in patients who fail 24-48 hours of conservative therapy and in those with a cecal diameter >12 cm. It can lead to bradycardia, bronchospasm, and hypotension and is contraindicated in those with certain cardiovascular risk factors (recent myocardial infarction, bradycardia, beta blocker therapy), active bronchospasm, or peptic ulcer disease (Choice B). Patients who fail neostigmine or have contraindications may require colonoscopic or surgical decompression, including a percutaneous tube cecostomy.